On June 15 Parkinson Society Southwestern Ontario (PSSO) hosted a webinar on Assistive Devices for Daily Living. Two Master’s Students in the occupational therapy program at Western University were the speakers. They began by explaining that the purpose of assistive devices and occupational therapy are to help people with limited or alternative abilities continue to do the task they need or want to do, whether that be self-care, employment/volunteering, or recreation.
Full Story>>
Before sharing tips and demonstrating several assistive devices to aid in dressing, meal preparation, and eating, they made the point that you cannot force someone to accept alternative ways to accomplish tasks. Instead, you must meet them where they are. While answering questions at the end of this webinar, the speakers suggested how to approach someone who may benefit from assistive devices.
The webinar can be viewed on the PSSO YouTube channel.
The Stanford Parkinson’s Community Outreach Program hosted a webinar on a similar topic of home care ‘gadgets’ in June 2021 and posted the recording the Stanford APDA YouTube channel.
In November 2021 we followed up the ‘gadgets’ webinar with a webinar on local resources families coping with PD would find helpful. That video is also available on the Stanford APDA YouTube channel.
And now, on with my notes…
– Denise
“Start Your Day in a New Way: Assistive Devices for Daily Living” – Webinar Notes
Speakers: Karlee Pringle, Master’s of Occupational Therapy candidate, Western UniversitySamantha Lau, Master’s of Occupational Therapy candidate, Western University
Webinar Host: Parkinson Society Southwestern Ontario (PSSO)
Webinar Date: June 15, 2022
Summary by: Denise Dagan, Stanford Parkinson’s Community Outreach
Learning Objectives
- Understand what assistive devices are
- Understand why assistive devices might be used
- Understand how an occupational therapist can support your participation in activities of daily living
- Learn about a variety of device options that support meal preparation, eating, and dressing
What is Occupational Therapy?
- A health profession that helps individuals regain or improve participation in the activities that they need to do want to do and are expected to do in a way that is meaningful to them.
- The term “occupation” is used to describe the activities that make up your day. These are categorized into:
- Self-care (dressing, bathing, eating, etc.)
- Productivity (working, volunteering)
- Leisure activities (what you do for fun!)
How can an Occupational Therapist Help?
- Observe how you currently complete tasks
- Provide strategies & help you develop skills that promote safety and meaningful enjoyment of activities
- Modify the environment or the task to facilitate safe and satisfactory participation
- Help you set goals for participation and support you in achieving those goals
Activities of Daily Living & Parkinson’s
3 Common Areas of Concern:
- Dressing: buttons, shoelaces, belts, overall balance while dressing
- Cooking: safety, preventing burns
- Eating: managing tremors, cutting food
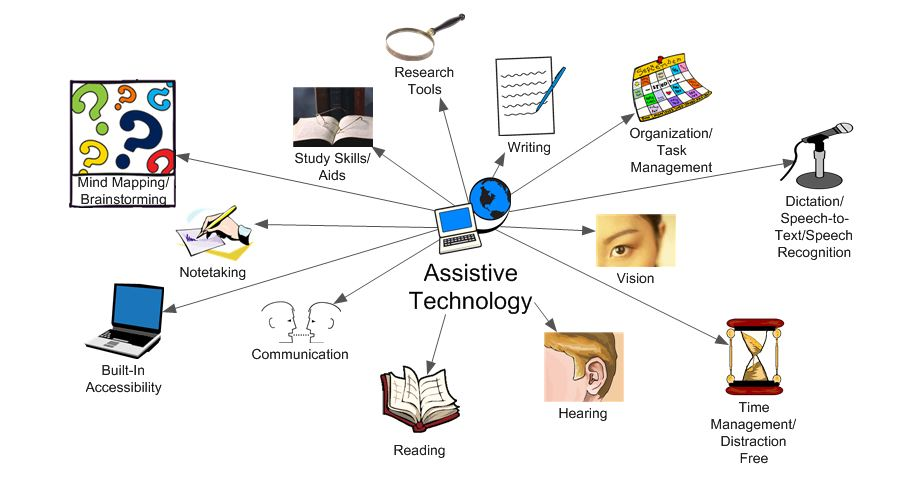
Introduction to Assistive Devices
Assistive devices are tools or “external devices that are designed, made, or adapted to assist a person to perform a particular task. People with varying abilities and disabilities may depend on assistive devices to enable them to carry our daily activities and participate actively and productively in community life.”
Assistive devices range from low tech (i.e., weighted eating utensils) to high tech (i.e., power wheelchair).
Why use assistive devices?
- Assistive devices support an individual’s ability to complete tasks in a way that is meaningful to them.
- It is important for those with PD to practice skills and continue to use them to extend the amount of time you are able to do perform those skills.
- Assistive devices can extend the amount of time you are able to perform skills.
- Promote safety
- PD issues such as dyskinesias, balance, tremor, orthostatic hypotension (dizziness) can make it difficult to complete tasks in a safe manner.
- Assistive devices can make it easier and safer to complete tasks in a safe body position.
- Encourage self-efficacy (autonomy and self-confidence)
- Assistive devices can aid someone with PD to continue dressing themself and perform other self-care. This fosters autonomy and independence.
Live Demonstration of Assistive Devices (All devices are available on Amazon and likely from medical supply retailers.)
Dressing devices
People with PD tend to experience more difficulty with lower body dressing due to a number of issues, including balance, rigidity, dyskinesia, or fine motor skills
1. Sock aid – Once you have the sock positioned on the sock aid device, use the straps to pull the sock onto the foot. The speaker described several designs of sock aid. This image is the type she demonstrated. Bunching up the sock to place over the end of the sock aid device requires fine motor skills.
Note: Sock aids for compression stocking are designed differently because the elastic in the sock is much tighter.

2. Shoehorn – acts as a slide to ease a shoe over the heel of the foot. Many people are familiar with short shoehorns (about 6 inches), commonly used by shoe salespeople.
The speaker recommends a longer shoehorn is recommended for those with PD, putting on shoes in a seated position (about 12 inches). This image shows the type of shoehorn the speaker demonstrated.

There are also much longer shoehorns for use while standing or for those who have difficulty bending forward while sitting.
3. Substitutes for shoelaces – Shoelaces can be challenging for those with PD because they require fine motor skills to tie. Bending over to tie shoes can also result in dizziness upon rising for those with PD who have orthostatic hypotension. These devices replace regular shoe laces so you can continue to wear your favorite lace-up shoes.
Coiled, elastic shoelaces – feed them through the shoelace holes as you would a regular shoelace. Some coil will be exposed on either side at the top of the row of holes. The shoelace will stretch when you put the shoe on (with a shoehorn) but relax back against your foot and hold the shoe on your foot securely.

Lock Laces – feed the straight (not coiled) elastic laces through the shoelace holes as you would a regular shoelace. Place your food in the shoe (with a shoehorn) and tighten the clasp until it feels secure and comfortable on your foot. Cut off any extra length.
Like coiled elastic shoelaces, Lock Laces will stretch when you put the shoe on (with a shoehorn) but relax back against your foot and hold the shoe on your foot securely.

4. Reacher/grabber – allows the user to reach for things without bending over, getting on tiptoes, or climbing to reach things overhead (any of which could lead to loss of balance and falls). Pulling the trigger causes the claw on the end of the device to close, allowing you to pick up things, particularly dropped articles of clothing.
Note: The speaker’s demonstration model had a joint in the middle of the reacher/grabber’s arm, which came disconnected. Perhaps purchasing a design where the arm is a single piece would circumvent that problem.
5. Zipper loop – Not an official product. Just add the ring part of a keyring to the end of a zipper pull to give someone with fine motor skills challenges a larger pull to hang onto or put a finger through to easily pull up the zipper on a jacket.
Meal Preparation Devices – for ease of use and safety
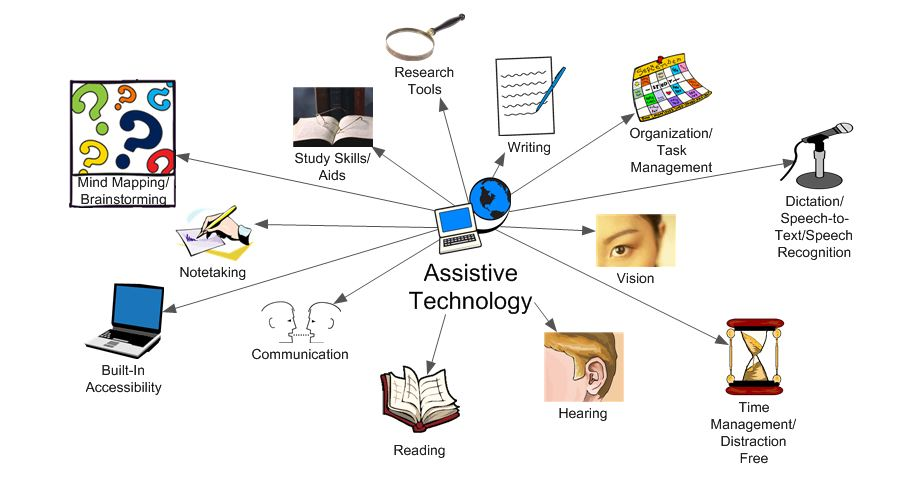
1. Adaptive Cutting Board – The speaker showed a cutting board designed with one corner having raised sides to push up against and two spikes in the center of the board to push items onto, so they don’t slide around. There are many design variations.
The speaker demonstrated putting a slice of bread into the corner so it will not slide while being cut in two to make half a sandwich. She then demonstrated piercing a carrot on the spikes so it doesn’t roll while being sliced.
2. Jar opener – place the jar lid onto the appropriate size hole in the jar opener and twist the jar opener. The jar opener can also be used to tighten lids onto a jar.

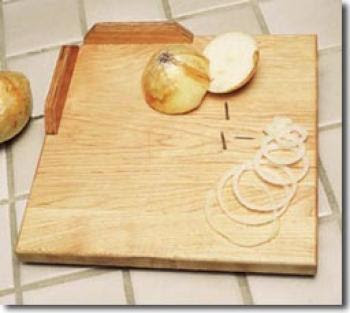
3. Rubber mat – anti-slip rubber or silicone material that can keep regular cutting boards, plates, and bowls from sliding around on counter or tabletop.
4. Kettle tipper – a wire frame that holds an electric hot water kettle with velcro. The frame tips to pour water into a cup without having to lift the kettle.
Note: The speaker did not mention how to fill the kettle… Many kitchen faucets have a wand feature. Perhaps this would be a useful item if the kettle with kettle tipper is kept by the sink and filled with the faucet’s wand, thereby requiring no lifting to make a hot beverage.

5. Kitchen timer – to remind you to return to whatever you’re cooking if you must step away and have issues with memory. Kitchen timers come in many varieties, both analog and digital. This is the type the speaker showed.
Eating Devices – to address issues like tremor and strength
Some people with Parkinson’s have diminished sense of smell with decreases taste and the pleasure of eating. Tremor and strength issues detract from the pleasure of eating even more. Recipes with strong flavors, along with these devices may make eating more enjoyable, help maintain weight, and combat malnutrition.
1. Rocker knife – allows cutting single-handed using a full grip, downward motion, and the strength and leverage of the entire arm. This can be used during meals in lieu of a knife and fork, which requires more fine motor control and hand strength.

2. Scoop plate (with or without suction cups on the bottom) – a plate with a raised lip all the way around, allowing one to scoop food against the lip to get food onto a spoon.
Note: If you happen to have a baking dish for quiches or pie pan with reasonably vertical sides, it will work equally well.

3. Scoop guard – plastic or metal side that attaches with clips to the rim of a regular dinner plate, allowing one to scoop food against the lip to get food onto a spoon.
The speaker suggested using the rubber mat under your plate if tremor causes the plate to slide around on the table.

4. Utensils – Many different options, including
Weighted utensils – looks exactly like regular utensils, but it is heavier, counteracting the motion caused by tremor but can cause fatigue in the hand and/or arm.
Built up handle utensils – the handles are usually plastic or rubber, while the bowl, blade, or tines are metal. These allow for a better grip for people who have a weak grasp or difficulty holding thin, regular utensils. Handles may be smooth and hard, ridged, or somewhat conforming to the palm.
Built up handle utensils can be:
- Weighted – heavier handle counteracts the motion caused by tremor but can cause fatigue in the hand and/or arm.
- Swivel – the metal bowl or tines swivels or wobbles in the handle. This can be good for those with dyskinesia or tremor because if the hand/handle shakes the food stays on the utensil.
- Angled spoon – the bowl of the spoon is bent to the side, allowing the user to keep their wrist straight while eating. This is useful for those with rigidity or restricted range of motion. Bent forks are also available.

5. Weighted cup – plastic cup with a weighted bottom and oval shape, which allows better control over the flow of liquid from the cup into the mouth.
Another option to control the flow of liquid into the mouth is using a straw. Either reduces the risk of choking due to too rapid flow of liquid into the throat.

Tips for Dressing
- Lay out the clothes you will be changing into before changing (e.g., on the bed)
- This conserves energy and prevents fatigue.
- Remain seated as much as possible
- Conserves energy and prevents fatigue
- Prevents falls
- Dress the more affected/weaker side first (if applicable)
- If needed, take a break before donning the other sleeve or leg.
- Dress during ON periods.
Tips for Meal Preparation
- Complete as many preparation tasks as possible in a sitting position (e.g., chopping vegetables, grating cheese, mixing ingredients)
- Conserves energy and prevents fatigue
- Ensure that regularly used items/appliances are in easy reach
- Store items used together in the same place (e.g., create a beverage station, baking needs near stand mixer, etc.)
- Conserves energy and precludes use of a stool, which could lead to a fall.
- Ensure that there is adequate lighting in your cooking environment
- Prevent fatigue, recipe mistakes, and injuries
- Allocate extra time to cooking to accommodate breaks
- Wipe up spills as soon as they occur
- Prevent slipping and falls
Tips for Mealtimes
- Take your time chewing and swallowing
- Avoid filling cups all the way to prevent spills, especially while walking
- Bring awareness to maintaining an upright position to prevent choking
Note: If you experience difficulties with chewing and/or swallowing, make sure to speak with your doctor. A speech evaluation may be warranted, followed by referral to a speech-language pathologist (SLP).
This is just the tip of the iceberg! There are as many assistive devices as you can imagine for the activities discussed today as well as for showering, bathing, grooming, toileting, and leisure occupations. See the attached lists of assistive devices and adaptive clothing from PSSO to see what options might work for you. To finer tune what assistive devices will work for you, consult with an occupational therapist.
Questions & Answers
Question. A webinar attendee asked where she could look at the utensils in person.
Answer. Get a referral to an occupational therapist (OT) because they often have sample utensils to try out. Also, consider buying from someplace like Amazon that allows free returns.
Question. The same attendee asked how to get a referral to an OT.
Answer. Ask your regular physician or neurologist for a referral to an OT, preferably one with experience working with those who have PD.
Question. The same attendee asked if OT is covered by insurance for those diagnosed with PD.
Answer. Yes, although some OTs with specialized training in treating PD may be private pay. You can submit the bill for private pay OT to your insurance provider.
Question. An attendee’s mother has PD, and she wants to remain independent. How do I approach her to ask if she would like to investigate assistive devices.
Answer. Occupational therapy talks about meeting people where they are and helping them find ways to be able to do the things they want to do. So, don’t push the issue. Rather, be tuned in to when your Mom needs a hand with certain tasks. That is the time to bring up the issue of OT and assistive devices.
Assistive devices are intended to facilitate independence. Researching assistive devices is how the two of you can work together to achieve her goal of maintaining independence for as long as possible. You are both on ‘team independence.’
