In mid-March, the UCSF Memory and Aging Center (MAC) offered a webinar on Lewy body dementia (LBD), featuring William Mantyh, MD, a UCSF neurologist who researches the genetic causes of various dementias. It was the first in an ongoing series about LBD. Dr. Mantyh provided an overview of LBD symptoms and diagnosis, including autonomic issues; explained our current understanding of the causes and risks; and outlined the available treatments. We at Stanford Parkinson’s Community Outreach listened to the webinar and are sharing our notes.
The webinar was recorded and is available on YouTube.
If you have questions about the webinar, you can contact the UCSF Memory and Aging Center at MAC@ucsf.edu.
“Lewy body dementia” is an umbrella term that includes dementia with Lewy bodies and Parkinson’s disease dementia. The UCSF MAC has a webpage on “dementia with Lewy body disease” and “Parkinson’s disease with dementia”:
For further information on Lewy body dementia, check out this list of resources on the Brain Support Network (BSN) website.
Now… on to our notes from the webinar.
– Lauren
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
What is Lewy body dementia and how is it treated? – Webinar notes
Presented by the UCSF Memory and Aging Center (MAC)
March 12, 2020
Summary by Lauren Stroshane, Stanford Parkinson’s Community Outreach
The speaker, William Mantyh, MD, is a neurologist with the UCSF Memory and Aging Center (MAC) who researches the genetic causes of Alzheimer’s disease and Lewy body dementia (LBD), which have similar underpinnings. He provided an overview of LBD symptoms and diagnosis, including autonomic issues; explained our current understanding of the causes and risks; and outlined the available treatments.
Lewy body dementia (LBD) is an umbrella term for diseases caused by the same abnormal protein, including Dementia with Lewy bodies (DLB) and Parkinson’s disease dementia (PDD). In DLB, cognitive symptoms occur within one year of the onset motor symptoms, whereas in PDD, cognitive symptoms lag behind motor symptoms by at least a year.
Overview of symptoms and diagnostic criteria
Each patient is unique; each individual may have a different set of symptoms, and symptoms may change or evolve over time.
Common symptoms in LBD:
- Visual hallucinations, often of people or animals, and usually non-threatening;
- “Supernatural” experiences, i.e. feeling the presence of someone nearby when there is no one there;
- Cognitive impairment, usually manifesting as difficulty with organization, multitasking, visuospatial tasks;
- Dream enactment behavior, or REM sleep behavior disorder (RBD), such as flailing arms and legs, yelling, screaming, or cursing during sleep, with a varied level of consciousness throughout the day, such as an irresistible urge to nap, or spacing out;
- Intense paranoia, depression, anxiety, delusions of family members being imposters (Capgras delusion);
- Disturbances of the “autonomic” nervous system (constipation, bladder spasms, erectile dysfunction;
- Parkinsonism, such as a stooped posture, tremor, stiffness, shuffling gait, slow movement, imbalance/falls, soft voice, and decreased facial expression.
There is no blood test or biomarker test to diagnosis LBD. The core criteria that a physician will use to give a diagnosis of LBD include fluctuating cognition with significant variations in the person’s level of attention and alertness throughout the day; recurrent visual hallucinations; and parkinsonism, such as slowed movement, tremor, and stiffness.
Other symptoms that make the diagnosis of LBD seem more probable to a clinical include severe sensitivity to antipsychotic agents, repeated falls, episodes of fainting or unresponsiveness, autonomic dysfunction (described below), excessive daytime sleepiness, decreased sense of smell, delusions, and apathy, anxiety, or depression.
What is autonomic dysfunction?
The autonomic nervous system handles a lot of the “automatic” functions of your body – things you don’t consciously think about, like regulating your blood pressure or digesting food. Autonomic dysfunction is when this system isn’t working normally, and can manifest as lightheadedness when changing position, abnormal heart rate, constipation, urinary incontinence or spasms, lack of sweat, and erectile dysfunction. Symptoms of autonomic dysfunction are common in LBD, and something to monitor for over time.
How does LBD typically progress?
LBD develops slowly, over years or decades. For some patients, early features of DLB or PDD may have manifested in their 30s as constipation, or acting out their dreams, decades before they later developed the cognitive signs of dementia.
Once a person has dementia, median survival is about 5 years. Progressive symptoms typically include worsening motor symptoms of parkinsonism, such as more falls, worse tremor, or greater difficulty walking. Visual hallucinations and delusions become more persistent. Eventually, swallowing difficulties usually occur, leading to pneumonia – the number one cause of death in LBD.
What causes Lewy body disease?
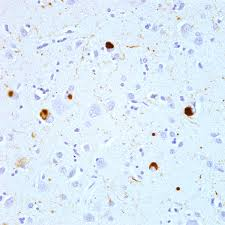
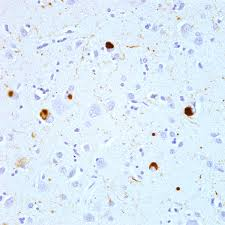
We don’t really know, but investigation is underway. Lewy body disease is associated with tiny deposits of the protein alpha-synuclein in the brain. Normally, this protein helps neurons communicate with one another, but in Lewy body disease, the protein forms abnormal deposits called “Lewy bodies.” Although we know that Lewy bodies are always associated with LBD, we do not yet know definitively if they are part of the problem or maybe an “innocent bystander.” They could even have a protective effect – we don’t know for sure.
Most cases of LBD have no known cause, though about 5 percent of cases of LBD are caused by a known genetic mutation. There is some evidence that exposures to certain toxins early in life may be risk factors for eventually developing LBD.
There are lots of possible risk factors that do not yet have conclusive evidence, including history of traumatic brain injury; vitamin D deficiency; history of migraine with aura; living in urban or industrial areas where copper, magnesium, and lead are common; exposure to hydrocarbon solvents; farming or agricultural work; consumption of well water; a diet high in iron and manganese; excess body weight and type 2 diabetes; higher levels of education along with a history of anemia; and lower muscle strength in late adolescence.
Genetic risk factors may involve the cell’s “garbage disposal system,” the cell’s ability to produce energy, and the correct or incorrect folding of alpha-synuclein.
Current treatment approaches
We do not yet have an existing treatment to stop or slow the progression of LBD, except one: physical exercise! Evidence shows that physical exercise not only slows the progression of the disease, but also lowers the risk for those who have not yet developed it. However, exercise can be a challenge due to the mobility issues caused by LBD, as well as problems with motivation. Finding safe modes of activity such as pool exercises or stationary cycling can be very helpful. Medications are often prescribed to help manage the symptoms of LBD: cognitive symptoms, sleep, anxiety & depression, and motor symptoms can sometimes be addressed.
Acetyl-cholinesterase inhibitors are the first-line group of medications used to improve alertness, hallucinations, and delusions; they include the drugs donepezil (Aricept), galantamine, and rivastigmine (Exelon). These medications do not help all LBD patients, and can cause side effects such as urinary frequency, gastrointestinal distress, and slowed heart rate.
If the first-line approach is not helpful, the second-line medications may be tried, but carry a higher risk of serious side effects. These include pimavanserin (Nuplazid), quetiapine (Seroquel) or clozapine (Clozaril). These medications carry a black box warning from the FDA that elderly patients with dementia-related psychosis who are treated with antipsychotic drugs have an increased risk of death.
Editor’s note: A previous version of this blog post stated that pimavanserin carries a black box warning due to the potential to cause a cardiac arrhythmia (QT prolongation), however, this is incorrect. The black box warning attached to pimavanserin is due to its classification as an antipsychotic, which carries an increased risk of death in elderly patients with dementia-related psychosis. We regret the error in the original post.
For sleep disturbances, the two main medications used in LBD are melatonin, which is a synthetic version of our body’s naturally-occurring sleep hormone, and available over-the-counter; and trazodone, an antidepressant that can also be very useful for sleep, but can also cause side effects of sedation, dizziness, dry mouth, and nausea.
Anxiety and depression are common in LBD, often arising long before a diagnosis has been made, and it is important to try to manage these symptoms since they can severely impact quality of life. Selective serotonin reuptake inhibitors (SSRIs) are a class of antidepressant that are often used in LBD, namely escitalopram (Lexapro) and citalopram (Celexa). They tend to carry mild side effects and are usually well-tolerated. They can cause sleepiness or gastrointestinal upset in some individuals.
For those who also have parkinsonian symptoms, carbidopa-levodopa (Sinemet) can be helpful to improve motor function by making it easier to move. It can cause side effects such as sedation, lightheadedness, worsening hallucinations or delusions, and impulsive behavior. Physical therapy can help to prevent falls, while “big and loud” speech therapy can improve speech volume and make it easier for the person to communicate.
Medications to avoid in LBD
The brains of people with LBD are deficient in dopamine, and some medications act on the brain to further block dopamine. If someone with LBD is given one of these medications, the brain becomes acutely deprived of dopamine, with potentially dangerous results – the person may become essentially unable to move. First-generation antipsychotics such as haloperidol (Haldol) or risperidone (Risperdal) fall into this category. Other medications that are sedating can worsen confusion or other cognitive issues, such as Benadryl (diphenhydramine) or some versions of Tylenol PM.
In case of hospitalization, it is good to know which medications should be avoided. If the hospitalization is anticipated, you can bring a list with you to provide to the inpatient team so they are aware to steer clear of these medications unless absolutely necessary. Your neurologist’s office likely has such a list that they can give you.
Non-medication / behavioral approaches
Aside from medications, there are other approaches that can be helpful for managing LBD symptoms such as agitation and delusions. Dr. Mantyh gave an example of a patient who became really agitated every time he went in the bathroom; it was difficult to bathe him or get him to brush his teeth. With some detective work, it turned out the mirror in the bathroom was upsetting to him. Once the mirror was removed, his behavior improved. Identifying what stimuli are provoking the person’s “bad” behaviors can go a long way to mitigating these episodes.
- Try to identify any preceding events prior to an episode of agitation, to figure out triggers for their behavior.
- Prevent or change the individual’s exposure to triggering stimuli or events.
- Try to avoid sudden changes in the environment, which can be disorienting for the person. If you need to travel, be prepared for more issues.
- As much as possible, stick to a routine sleep-wake cycle, with exposure to plenty of natural light in the morning. Avoid fluorescent or backlit screens for several hours before bedtime, as these can confuse the brain.
- Playing the person’s favorite music or spending time with a pet can be soothing.
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Question & Answer Session
Q: How can I find clinical trials that are exploring LBD, genetic risk factors, or potential treatments?
A: There are a number of different resources to help you get involved in research. You can search by diagnosis, location, or what type of trial interests you – for instance, is it a trial testing out a new drug, is it trying to understand the disease better, is it evaluating imaging?
The website ClinicalTrials.gov from the US National Library of Medicine is a useful resource for clinical trials. It is searchable using multiple different criteria, including trials that are actively recruiting now.
The Michael J. Fox Foundation Trial Finder is a good resource for searching current clinical trials related to PD.
Lastly, Dr. Mantyh recommended the Alzforum, a blog which is geared towards Alzheimer’s disease but has a lot of accessible summaries regarding research or other topics relevant for those with other neurodegenerative diseases.
Q: Is a GBA mutation a risk factor for developing inherited LBD?
A: This is a cutting-edge question these days. The glucocerebrosidase (GBA) gene is a key “garbage man” of the brain, helping clean things out. If you get two “bad” copies of this gene, one from each of your parents, you end up with Gaucher’s disease, in which the lysosomal storage systems in the cell don’t work normally and the body is unable to process certain types of fats, which then accumulate dangerously in the body. These patients typically die very young.
If you get one “bad” copy of the GBA gene, you do not get Gaucher’s disease. But you are at increased risk for developing neurodegenerative illness, such as Parkinson’s disease (PD). There are a lot of studies that are spawning around these questions about GBA mutations, but we do not yet know if a GBA mutation can lead to inherited LBD.
Q: I have several first-degree relatives with Alzheimer’s disease, DLB, and PD. Is there anything I can do to explore my risks?
A: You can certainly get screened for known genetic mutations in a clinical research setting, but in Dr. Mantyh’s experience, they often come back negative, even for those who have a strong family history. There is a lot we don’t know yet about the genetic mutations that may predispose someone to developing these illnesses – there are likely other mutations out there that we just don’t know about yet.
Q: Do we have evidence that exercise can reverse the disease?
A: Unfortunately, we do not have evidence that anything can reverse the disease process in LBD. It does progress over time. However, it is pretty rare for someone who is ill with LBD to have no other illnesses at all. Targeting other health factors such as smoking, a sedentary lifestyle, unhealthy diet, can improve their overall health and may even help their cognition. It won’t stop the progression of LBD, but it can still positively impact their ability to think well.
Q: I am a caregiver for someone with LBD who sleeps 20 hours in every 24-hour period, napping most of the day and also sleeping through the night. What strategies or medications might be useful in this circumstance?
A: The first thing to look at is what medications are they on? Sinemet (carbidopa-levodopa) can improve the speed of one’s movements but can also cause drowsiness. It can be a balancing act to get enough medication on board while not being too sedating. What other medications are they on? Narcotics for pain or benzodiazepines to help with sleep can also make someone sleepy.
Try to keep the person as engaged as possible, in a brightly lit room; simple activities or visits from family members can be helpful.
Lastly, obstructive sleep apnea (OSA) is common in LBD and can make someone feel exhausted all the time. If there is any concern that their airway is closing up – such as loud snoring, coughing, gasping, or choking during sleep – then getting evaluated for OSA is a good idea.
Q: Is there any correlation between heavy alcohol use and risk for DLB?
A: There isn’t any known link between alcohol abuse and DLB. However, someone with LBD will be more severely affected by alcohol. Those with chronic alcohol abuse can have some shrinkage in the cerebellum, and may also have decreased cognitive reserve – their brain is already handicapped. When you add on Lewy body disease, they may suffer more severely from cognitive impairment.
Q: What is the average time from onset of symptoms to getting a diagnosis?
A: We don’t have numbers on how long it typically takes for a diagnosis. It can be very difficult to know if certain signs, such as constipation or lost sense of smell, are evidence of LBD or just present on their own, and there haven’t yet been many studies looking into this question. The general consensus is that it takes decades to spread.