In early August, the APDA (American Parkinson Disease Association) Massachusetts hosted a webinar on how blood pressure changes can have an impact on Parkinson’s disease (PD). The speaker, movement disorder specialist Anindita Deb, MD, gave an overview of neurogenic orthostatic hypotension (nOH) and described medications and non-pharmacological treatments. Here are our notes from the webinar.
The question-and-answer session with Dr. Deb was particularly interesting. Here’s the first question and answer:
Question: My doctor says I should eat small meals frequently. Why is that important?
Answer: When you eat and digest your food, it requires blood flow to be directed to your gut, so it helps you digest. Sometimes, when you eat too much, there is too much blood flow to your gut which makes you feel lightheaded. If you have smaller, more frequent meals, then it does not require so much blood flow in your stomach and that may mitigate your symptoms rather than having a large meal. Also, it helps digest the food more regularly as you may have motility and gastric slowing symptoms with Parkinson’s. Smaller meals will help the gut process the food slowly each time.
The webinar was recorded and is accessible on the APDA’s YouTube page.
Stanford Parkinson’s Community Outreach Program also has relevant information on its orthostatic hypotension webpage.
See notes below for all the details.
Regards,
– Sheela Sakariya
Understanding Blood Pressure Fluctuations
Webinar Host: APDA Massachusetts
Webinar Date: August 10, 2021
Summary by: Sheela Sakariya, Stanford Parkinson’s Community Outreach
Speaker: Anindita Deb, MD, movement disorder specialist, University of Massachusetts, School of Medicine, Worcester, MA
Overview
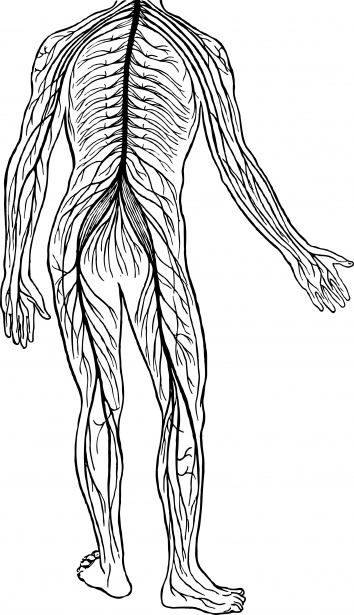
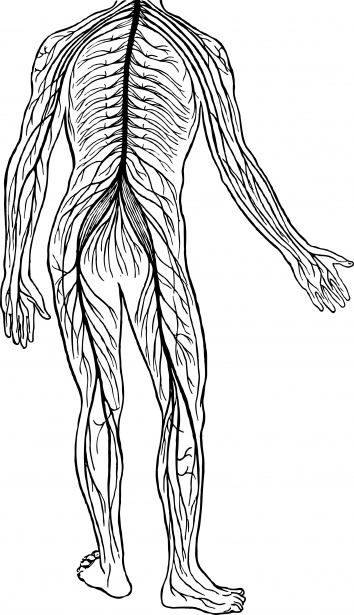
Blood pressure (BP) is:
- Controlled by central autonomic nervous steam (controlled by the brain)
- Regulates heart rate, blood pressure, digestion, urination, sexual function
- Controlled by peripheral autonomic nervous system (controlled by the peripheral nerves)
The peripheral autonomic nervous system includes:
Sympathetic system
- Fight or Flight: emergencies, exercise
- Multi organ innervation
- Epinephrine and norepinephrine mediated
- Smooth muscle, cardiac muscle, and glands
Parasympathetic innervation
- “Rest and digest; “ conserving energy
- Localized effect
- Acetylcholine mediated
Autonomic Dysfunction in Parkinson’s Disease
Orthostatic hypotension (drop in BP) is very common. Also called neurogenic orthostatic hypotension (nOH) in the context of PD.
Other autonomic symptoms include
- Constipation
- Urinary symptoms
- Sweating
- Drooling
- Sexual dysfunction
Orthostatic Hypotension (OH) — Definition and Symptoms:
Sustained reduction in systolic blood pressure by 20mmHg or diastolic by 10mmHg within 3 mins of standing or head-up tilt (title table testing)
Symptoms: fainting, lightheadedness, dizziness, neck pain, nausea, sweating, blurry vision, confusion, thinking, and memory difficulties.
Exacerbated in the morning, after meals or in heat.
How to test/monitor for nOH:
Take your blood pressure lying, sitting and standing about 1-3 mins apart
If there is a 20-point difference between the top numbers OR a 10-point difference in the bottom numbers on changing position, then this meets criteria for OH
Other testing:
- Autonomic testing including a tilt table test
- Tilt table test: lie on a table which will be gradually tilted up 10 degrees at a time to 70-degree tilt with measurements in BP/HR with each increase. (HR = heart rate)
Medications can affect blood pressure
Levodopa can decrease your baseline blood pressure
Many hypertensive patients can eventually lower or discontinue their blood pressure medications
Some medications such dopamine agonists (ropinirole, pramipexole), and selegiline can worsen nOH as well
Medications to lower blood pressure (anti-hypertensives) can exacerbate nOH so these should be discussed with neurologist and primary care physician/cardiologist and BP should be monitored closely. Examples: metoprolol, lisinopril, furosemide (lasix), amlodipine
Treatment of nOH
- Check sitting and standing BPs at every office visit (and at home if directed)
- Hydration 60-80 oz/day
- If on anti-hypertensive, re-evaluate need for this
- Consider changing timing of anti-hypertensive to late morning/afternoon or evening after discussing with PCP/cardiologist
- Compression stockings – wear these daily
- Abdominal binder – if having significant symptoms
- Add salt to die (depending on cardiac fix)
- Discuss with neurologist about reducing levodopa dose or reducing doses of other dopaminergic medication
- Discuss the need for medications to treat nOH
Recommended Physical Maneuvers
[Editor’s Note: The speaker showed this slide of six physical maneuvers.]
Medications
Midodrine
- Peripheral agonist
- Vasoconstriction
- Dose: 2.5-15mg (morning, noon, afternoon)
- Side effects: pupillary dilation, piloerection, paresthesias, pruritus, supine hypertension (avoid bedtime dosing)
Fludrocortisone (Florinef)
- Is a mineralocorticoid
- Expands intravascular volume, reduces salt loss
- Dose: .1-.3 mg/d
- Risk of volume overload, and hypokalemia or hypomagnesemia
- Additional side effects: headache, edema, weight gain, and supine hypertension
Droxidopa (Northera)
- Norepinephrine prodrug – neurogenic orthostatic hypotension
- Dose: 100-600mg TID
- Phase III trial of 100-600 mg TID droxidopa over 8 weeks showed improvements in standing BP, symptoms of lightheadedness and most notably 50% reduction in falls reported.
- Side effects: supine hypertension, headache, dizziness, nausea, fatigue
Pyridostigimine (Mestinon)
- Enzyme inhibitor
- Dose: max 60 mg TID
- Significantly improves standing BP in patients with OH
- Does NOT worse supine hypertension
- Effective alone or in combination with midodrine
- Side effects: diarrhea, salivation, nausea, vomiting, muscle cramps, fasciculations
Q&A Session
Question: My doctor says I should eat small meals frequently. Why is that important?
Answer: When you eat and digest your food, it requires blood flow to be directed to your gut, so it helps you digest. Sometimes, when you eat too much, there is too much blood flow to your gut which makes you feel lightheaded. If you have smaller, more frequent meals, then it does not require so much blood flow in your stomach and that may mitigate your symptoms rather than having a large meal. Also, it helps digest the food more regularly as you may have motility and gastric slowing symptoms with Parkinson’s. Smaller meals will help the gut process the food slowly each time.
Question: Do you think it’s a good idea to check your BP at home from time to time?
Answer: It really depends, and it’s a discussion between the patient and the neurologist. Not everyone develops the symptoms of orthostatic hypotension, so I don’t think it’s necessary. We also often don’t want the patient too focused on the numbers; we want to focus on the symptoms. Getting anxious over numbers can perhaps cause more anxiety and other symptoms, so unless you are directed by a physician to monitor your numbers, you generally don’t need to do it regularly.
Question: Do you have any tricks on how to drink more water during the day?
Answer: I usually recommend a sports water bottle that measures how much you drink, and having that with you wherever you are going. Or maybe if you are home, keeping one in every room that you will be in, so it reminds you to keep drinking water. Often, even if I don’t have water next to me, I will forget to drink.
Question: I hear the phrase “white coat syndrome” as it relates to blood pressure. Can you explain what that means?
Answer: White coat syndrome is essentially when you come to see your physician in the office, blood pressure tends to shoot up then you normally might be at baseline. That might be because there is some anxiety about going to the doctor’s office, and you may also be rushing to get there. That’s the reason we can’t rely solely on the BP readings we get at the office to diagnose orthostatic hypotension. It’s always good to have numbers from home or your natural environment in actual day to day and to see if you are really dropping.
Question: How many times a day should the lay-sit-stand blood pressure be taken?
Answer: Different physicians may have different preferences. I would go by with what your physician recommends. I would generally start with twice a day – first thing in the morning and then in the afternoon. And then if there is suspicion/symptoms, then the physician might add another check in time after medication/mealtime.
Question: How much does coffee raise blood pressure generally?
Answer: Coffee does raise blood pressure; don’t know the exact amount. It’s going to be transient so it will not be full effect through the day.
Question: Any data about hypotension after swimming?
Answer: Not that I know of; I have not seen blood pressure drop after exercise. In general, it might go up slightly or not change that much, but I would not assume it would drop after swimming.
Question: Please discuss orthostatic hypotension with supine hypertension as it relates to Parkinson’s disease.
Answer: Orthostatic hypotension is when blood pressure drops as you change position. Supine hypertension generally occurs as a side effect of the medications I discussed where those medications cause changes physiologically to your body to increase blood pressure. We also know that a maneuver like laying down increases blood pressure; so now if you are laying down and taking medications to increase BP, it might just push it up too high and that’s called supine hypertension.
Question: What is the cutoff for safe systolic/diastolic blood pressure in view of falls if no symptoms?
Answer: Everyone lives at a different number – what might be safe for me might be different for you and it really depends on your baseline. Generally speaking, I would like to see the top number (systolic) to be 90+ especially when you are standing. The diastolic numbers are hard to control even with the blood pressure medications; often I refer to my cardiology colleagues if the diastolic numbers are too high.
Question: Can shortness of breath and tightness of chest be a symptom for orthostatic hypotension?
Answer: Not the most common symptoms for orthostatic hypotension, especially if there is no lightheadedness and dizziness. You can have those symptoms in an OFF period, and the medication is wearing off. Talk to your physician and see if your symptoms correlate with orthostatic hypotension
Question: Should you wear long or short compression socks when you have trouble with blood pressure?
Answer: It really depends on the degree of hypotension. For my patients that are mild, I might recommend the short ones. I usually recommend the knee ones, as they are easier and more comfortable to wear. However, if you are having severe hypotension, then the thigh highs might be more appropriate. Talk to your physician to see what makes more sense for your symptoms.